future health africa:
QUALITY IMPROVEMENT & LEADERSHIP
OVERVIEW
Latest news
Our 2- year project funded by a UKAid SCCF grant is well underway. It is being delivered in partnership with LVCT Health, Kenya. It is focussing on helping Community Health Units (including Community Health Volunteers and Workers) in Migori and Laikipia Counties to improve pregnancy outcomes by encouraging mothers to engage with ante-natal clinics and skilled birth attendants.
The ‘learning event’ in Laikipia in April 2022 showed just how well CHVs and CHAs can adopt QI and leadership skills to help them in their work. It was very well supported by county and sub-county personnel and they all have action plans to deliver by the end of the project in November 2022.
https://www.ukaiddirect.org/news/14-charities-receive-small-charities-challenge-fund-grants
The award was for £48,781 and will run until November 2022.
What is q4a?
There is world-wide demand to improve quality in healthcare and this requires not only clinical expertise but also substantial improvements in systems of care. In other words we need to improve ‘sick systems’ as well as ‘sick patients. Despite substantial international funding, it is now recognised that improvements in healthcare systems won’t happen until health professionals themselves have the skills to lead the changes needed.
q4a runs programmes such as SPRINGBOARD which empowers frontline healthcare workers to improve their systems and their quality of care by learning and applying ‘The Science of Improvement’ and the ‘Art of Leadership’.
We believe that learning how to make sustainable change requires a combination of skills; knowledge of improvement methodology, team working, leadership, patient-centred care and an understanding of how to create a positive culture for change. We also believe these skills must be learned through doing real live quality improvement (QI) projects.
About to deliver the first SPRINGBOARD course in Nanyuki 2015
WhAT is q4a?
q4a (quality for all) is a group of committed healthcare professionals within the Future Health Africa charity who share a passion for improving the quality and safety of healthcare across the world.
We learned through working on clinical projects in Kenya since 2010, that ‘system’ problems are a huge contributor to poor patient outcomes but there were few opportunities for health workers to acquire the skills they need to tackle these. We formed q4a to address this gap and created the SPRINGBOARD* programme. It is designed to align with national policy on quality in healthcare (in Kenya, the Kenya Quality Model for Health - KQMH).
The q4a faculty teaching the SPRINGBOARD programme is made up of healthcare professionals from the UK and Kenya who have national and international expertise in:
Healthcare & Health System Strengthening
Quality Improvement, Innovation & Leadership
Coaching & building teams
Global Health
Partnerships
Education
International Health Consultancy
*original concept Dr Simon Knowles
WHAT DOES q4a DO?
Patient identification: another WHO priority, and one of our first q4a projects. Nanyuki, 2015
We share our skills in Quality Improvement and Leadership in order to contribute to advancing high quality, safe & efficient healthcare to accompany UHC. We believe that organisations and individuals need to adopt the culture and practice of continuous quality improvement (CQI) and the philosophy of patient-centred care. We run courses, support the QI projects that arise from them, assist with policy and participate in educational events. Our work is equally applicable in high and low-middle income settings.
We liaise with the Department of Quality & Standards in the Ministry of Health in Nairobi to share understanding of the impact of our training.
Overview
To demonstrate QI and leadership skills as they can be practised by any member of staff, we developed the interactive, enjoyable Springboard programme, a 10 day course delivered in 2 parts (Foundation & Advanced), each of 5 days, delivered a few months apart. We teach skills in QI methodology (a blend of ‘Lean’ and the Institute of Healthcare (IHI) ‘Model for Improvement’) and generic leadership skills. The courses empower individuals and teams to make real improvements that benefit both patients and staff in the places where they work. Teamwork, patient-centredness and a culture for improvement are emphasised throughout.
Skills are learned through doing QI projects LINK to QI projects below which we then support as requested.
We are developing a Train the Trainers programme so that we can build Kenyan faculty to deliver the course.
The programme was developed with the aid of grants from UKAid/the Department of International Development, administered by THET (Tropical Health & Education Trust).
Donations for Quality Improvement & Leadership “Quality for All” can be made at kind link at https://donate.kindlink.com/Future-Health-Africa/4943
Handwashing: a WHO priority…and one of our first q4a projects. Nanyuki, 2015
Courses (see below)
q4a currently runs 2 courses: Springboard Foundation and Springboard Advanced.
Both courses consist of a highly participative 5 day course of blended theory and practice. The courses are designed for delivery to healthcare professionals of all disciplines and are applicable to all levels of experience.
Course participants design and implement real quality improvement (QI) projects of their own choosing. They therefore acquire reusable QI methodology, leadership & team skills to empower them to further transform care within their health system. Post course mentorship from the Springboard faculty is offered and is tailored to the needs of individual course participants and that of their QI projects.
The Foundation Course focuses on QI methodology and project start-up with some tam and leadership skills. LINK to detail of Springboard Foundation course below
The Advanced Course, delivered 3-6 months later, teaches further leadership skills to help embed change. This is leadership for ALL, not just for people in leadership roles.
Springboard’s courses make Continuous Quality Improvement (CQI) ‘real and alive’ as the science of improvement and the art of leadership are taught through ‘doing’.
Listen to what one of our first participants, Grace Karoki, a Paediatric Ward Sister, has to say about the programme.
Grace Karoki, Paediatric ward sister and emergent QI coach talks about how the Springboard QI and Leadership programme is helping her hospital to improve patient care.
Maternity ward sister Charity talks about how they have improved pain relief after delivery for mothers in Nanyuki Teaching & Referral Hospital through a project set up through the Springboard QI and Leadership programme
Springboard Foundation Course
Overview
This course predominantly teaches quality improvement methodology and real projects are initiated to bring these skills to life. The methodology taught is a blend of the Institute for Healthcare ‘Model for Improvement’ and ‘Lean’ (Toyota Production System). Some leadership topics are introduced.
Objectives
Participants work in mixed cadre teams to identify a problem and create and sustain their own live improvement project to solve it. Having learnt how to do this with one problem, they should then be able to reapply the skills to other challenges in their facility.
Specifically, by the end of the 5-day course, participants will:
understand the principles and history of quality improvement generally worldwide and in their country
be able to apply the principles of 5S, the A3 worksheet and a driver diagram
be able to apply major QI analytical tools : problem definition, value stream mapping, identification of “waste”, root cause analysis (5 Whys, Pareto, fishbone etc)
appreciate the importance of data and measurement in improvement projects
be able to produce ‘run charts’ for presentation of data
understand ‘process’ tools such as the PDSA cycle and ‘huddles’
know the relationship between the science of improvement and the art of team & individual leadership
understand their personal learning and leadership preferences as individuals and within teams
Course Content & Structure (subject to variation)
Day 1:
Introduction to some of the principles of quality and patient safety.
Identification of a real facility-based QI project to work on. Prioritisation.
Formation of QI teams; how to build teams; understanding personalities at work.
Introduction to the A3 worksheet and tools that will be used to progress chosen QI projects.
Day 2:
Understanding the current problem and who needs to be involved in solving it.
Understanding 5S, waste and systems thinking.
Introduction to patient flow, capacity and demand.
Introduction to analysis tools.
Teams and facilitators go into the health facility for their first ‘Go See’ exercise.
Resuscitation analysis, Nyahururu, 2015
Day 3:
What do we want the future to look like and how could we get there?
Introduction to Innovation and reverse brainstorming.
PDSA cycles.
Understanding measurement for improvement.
2nd practical session on site.
Day 4:
Designing a test of change and the measures to be used.
3rd practical session and implementation of the first ‘test of change’.
Understanding challenges, roadblocks etc.
Day 5:
Engaging others in the change; communication through storytelling and data.
Presentation to senior managers
Design of next steps and strategies for sustaining progress.
Eligibility Criteria
Healthcare professionals of all disciplines and levels of experience can attend the Foundation Course. Support from participant’s direct supervisors / managers is essential as a crucial component of the course is the completion of a local quality improvement project.
Springboard Advanced Course
Overview
The Springboard Advanced Course revisits the projects established during the Foundation course and focusses on the leadership skills required to implement change. It promotes recognition of the fundamental importance of teams, leadership, empowerment and communication in building quality care. It starts to build the capability to coach others.
Objectives
Projects started during Springboard Foundation Course are revisited and progress is assessed. The course then teaches the skills required to advance their projects and manage challenges.
Specifically by the end of the course, participants will have learned how to increase their personal and team effectiveness through understanding themselves, the management of change, how to be effective and how to motivate others.
Course Content and Structure (subject to variation)
Day 1:
Teams present QI project progress highlighting successes and challenges.
Revision of tools used for measuring quality improvement.
Introduction to Myers Briggs personality groups.
Day 2:
Introduction to leadership and leadership styles.
Introduction to Covey’s Seven Habits of Highly Effective People.
Managing change.
Revision of effective ways of giving and receiving feedback.
Participants develop their own personal learning goals.
Day 3:
Introduction to emotional intelligence.
Introduction to coaching and mentorship.
Practical sessions to practice and received feedback on coaching and mentorship behaviours.
Time management skills.
Principles of delegation introduced and practised in groups.
The Medical Superintendent at Nyahururu Hospital discusses the overprescribing of antibiotics and other drugs by injection and how to tackle this important problem.
Day 4:
Introduction to and practical application of Seven Step Change Model & The Change Curve.
Exploring values, attitudes, behaviours and beliefs.
Discussions on creating and sustaining effective team.
Next stage planning.
Day 5
Applying skills learnt it to real issues.
Managing challenging relationships.
Presentation.
Eligibility Criteria
Healthcare professionals of all disciplines that have completed Springboard’s Foundation Course can attend the Advanced Course.
Comprehensive workbooks are provided for participants on both courses. Contact info@futurehealthafrica.org if you would like access to these.
QI PROJECTS
Quality Improvement (QI) & Leadership skills acquired on Springboard courses have enabled healthcare workers in both UK and African countries to improve healthcare quality through running effective QI projects. Each Foundation course generates 2-4 new QI projects. Here are some examples:
1. Improving handwashing (WHO priority)
2. Labelling all patients on admission (WHO priority)
3. Improving paediatric drug administration
4. Improving triage in the Emergency Department (ED)
5. Improving waiting times in the Emergency Department
6. Improving time to site intravenous infusions and therefore treatment on ward
7. Reducing fasting times for children waiting for surgery
8. Improving nursing care records to improve patient care
9. Improving internal referral processes to speed up diagnosis and reduce wasted resources
10. Reducing pain after childbirth
11. Improving triage in ED
12. Reducing inpatient parenteral injections - including antibiotics
13. Reducing outpatient parenteral injections
14. Reducing unnecessary waits for lab tests
15. Improving fasting times for adults waiting for surgery
16. Reducing cross-infection through better ward organisation
17. Reducing waiting times in the out-patient/emergency department
18. Improving resuscitation in the hospital
19. Improving communication
20. Improving clinic flow
PROJECT 1. Improving hand washing to reduce infection
Nanyuki Hospital seniors wanted to reduce hospital-acquired infections but staff engagement in hand-washing had proved difficult, not least because there was often no water or soap or antiseptic gel on the wards.
The Medical Superintendent Dr Kilonzo and his team were shocked by the reality of the lack of handwashing when they did a personal observation on a ward at the start of the SPRINGBOARD course.
They broke the problem down into its component parts and pressed for a better water supply, soap, gel and notices to be distributed. They reinforced this with hospital-wide teaching.
The team then came up with the innovative idea of raising the profile of handwashing for everyone by establishing two sinks with running water at the entrance gate to the wards, to be used by staff and visitors. They are well used. We have heard that another hospital has adopted this having seen what Nanyuki has done!
Now they are in line with the WHO priority to improve handwashing. The inclusion of the County Government Infection control person on the team proved very helpful and has enabled the lessons to spread to other facilities.
PROJECT 2. Labelling all patients on admission to hospital
(WHO priority)
Patient safety is severely compromised when patients can’t be correctly identified. Sick patients who are not fully conscious or confused are particularly vulnerable. It is best practice, reinforced by the WHO, for inpatients to wear an identity bracelet to avoid errors in drug administration, wrong site surgery and misplacement of babies with the wrong mothers.
The team worked to identify a process that would ensure that labelling could happen, arranged for bracelets to be provided and educated staff themselves on the wards.
Labelling has improved from the original <10% of patients to almost 100%. It is now just routine practice. Dr Panga, who was part of this team, is a strong advocate for patient safety and our lead for q4a in Kenya.
PROJECT 3. Improving paediatric drug administration
Sister Grace Karoki runs the Paediatric ward at Nanyuki Hospital. She wanted to improve prescribing on her ward. She had observed that difficulties in calculation of correct doses of drugs requiring injection was causing delays in sick children receiving their drugs, or incorrect doses or failure to administer them, resulting in the children’s conditions getting worse. It also meant that a qualified nurse (often the only one on the ward) was taking 4½ hours to do a drug round - and immediately having to start the next.
A calculation chart, cheap calculator, adaptation to the drug chart (to show mls as well as mgs) and ward education resulted in a dramatically better situation with all medications being given correctly and the drug round time reducing by more than half.
The pharmacist on the team made implementation of an amended drug chart and the dosage calculation chart quick and easy. Karoki’s meticulous measurement made her successful in the submission of a poster to the International Forum in Quality & Safety in Healthcare in London and it received a commendation. She and two others attended the three day conference. Karoki has gone on to make many more improvements on the ward and now acts as a coach for other new projects in the hospital.
PROJECT 4. Improving triage in the Outpatient/Casualty/Emergency Department (ED)
In most low to middle income countries (LMICs) where there is limited primary care availability, all manner of complaints and ailments arrive at the doors of an ‘outpatient’ or casualty department. Many hospitals do not have anything recognisable as an ‘Emergency Department’.
As a consequence, everything arrives at the same door - from a mild fever to a major road traffic accident. Good triage processes are essential to ensure that those in need of urgent treatment are seen as soon as possible.
Nanyuki & Nyahururu hospitals do have Emergency Departments but they are physically separated from the ‘outpatient’ department presenting both opportunity and challenge. In both hospitals teams have worked very hard to create better triage systems and reduce times to be seen. These are really complex issues requiring ongoing work. Triage has improved in both places since they started to review it.
PROJECT 5. Improving waiting times in the Emergency Department
Linked to better triage is the overall challenge of waiting times. Patients have to visit National Hospital Insurance Fund (NHIF) offices, medical records departments, multiple paypoints, labs, radiology, pharmacy and other places. Few patients leave without a long wait and the sicker ones deteriorate while they wait.
The problems can seem too big to tackle but using QI methods, the task can be broken down. Following some individual patients during their journeys provides information previously unseen by health professionals.
This is an issue which will require continuous attention over long periods of time, not least because workloads and systems around this department change over times and always will. However, this initial period when sick patients arrive is critical for survival and should command the kind of attention these teams are giving to their local issues. A project which will never finish! A good 5S process has already tidied up the departments and enabled more rooms to be released for seeing more patients more quickly.
PROJECT 6. Improving time to site intravenous infusions and therefore treatment on wards
Dr Simmel Karbolo presented his team’s project with other hospitals at the iSpeak conference. A good 5S process on the ward resulted
in much faster times to establish intravenous lines, enabling treatments to start much faster.
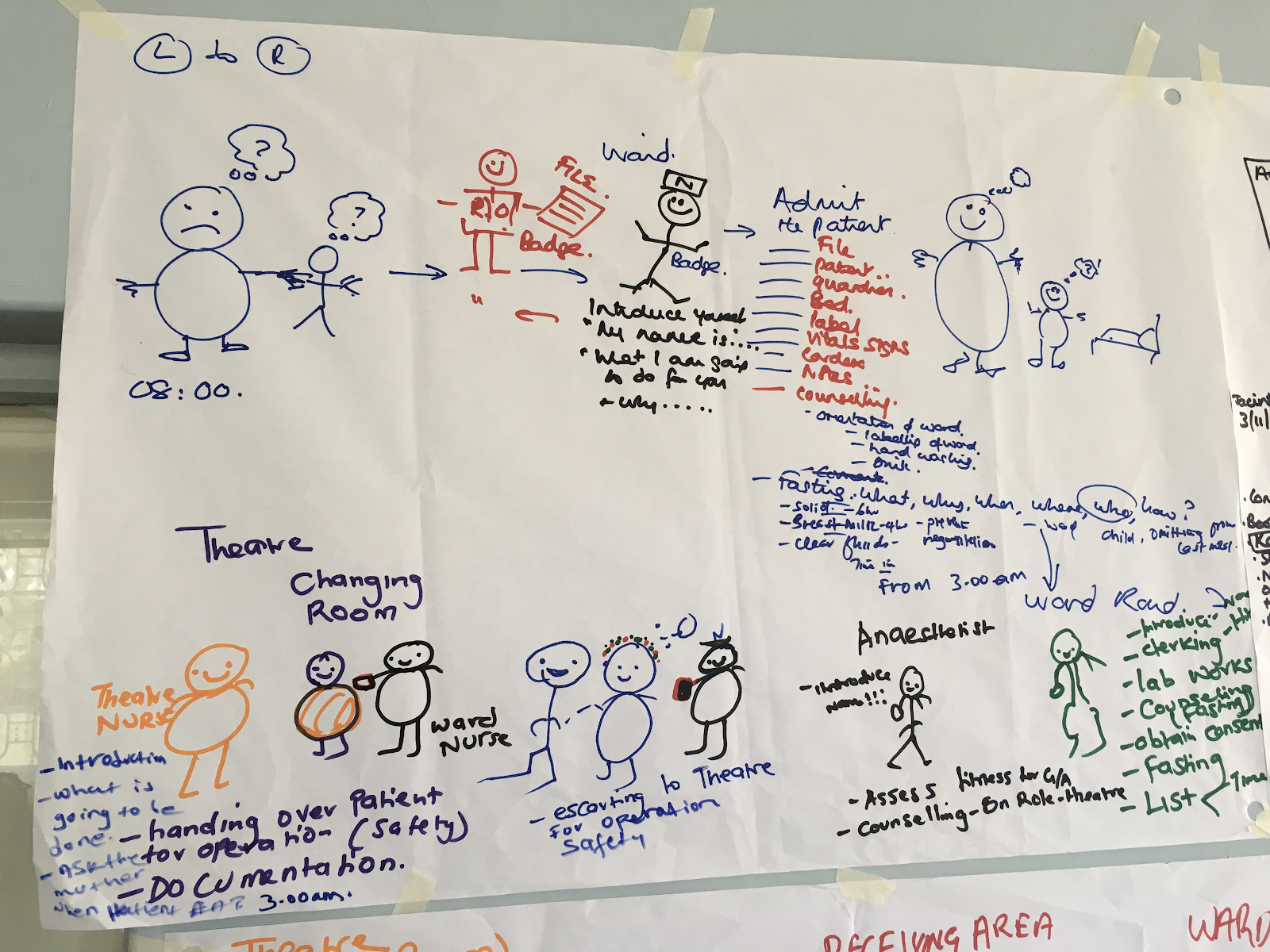
PROJECT 7. Reducing fasting times for children waiting for surgery
Ward nurses were unhappy as they felt fasting times for children before surgery were very long. They took a detailed look at the problem and realised that action had to be taken. After unpicking the problem in detail until they really understood it, they started to map out how things should be - and then made plans of how to create this better scenario. Among other changes, they implemented a new fasting time strategy and supported the change with posters on the ward and hospital-wide education.
PROJECT 8. Improving nursing care records to improve patient care
New Nursing Officer Wilson Kitonga wanted to improve the keeping of nursing care records in the hospital. This project started with one ward and having succeeded there, will spread the improved practice across other wards in the hospital.
PROJECT 9. Improving internal referral processes to speed up diagnosis and reduce wasted resources.
Patients needing radiological investigations were often incorrectly prepared, resulting in cancellation of the appointment. In turn this resulted in delayed diagnosis and much wasted time for the patient and radiologist. Improved patient and ward information has greatly improved this.
PROJECT 10. Reducing pain after childbirth
The Maternity ward had been receiving complaints about poor management of pain after deliveries of all types and wanted to tackle this. They were realising that it was resulting in babies being admitted to the NewBorn Unit because the mothers were unable to feed their babies satisfactorily. They have done this by changing the location of paracetamol and ibuprofen supplies and routinely giving these within one hour of the birth. (Caesarean Section patients receive morphine).
Since implementing this policy, complaints and NBU admissions have reduced hugely.
See nurse Charity talking about this project - which was relatively simple, fast to implement, cost nothing but has had a big impact.
PROJECT 11. Improving triage in ED
See projects 4&5 - these projects in a second hospital share the same experiences as above
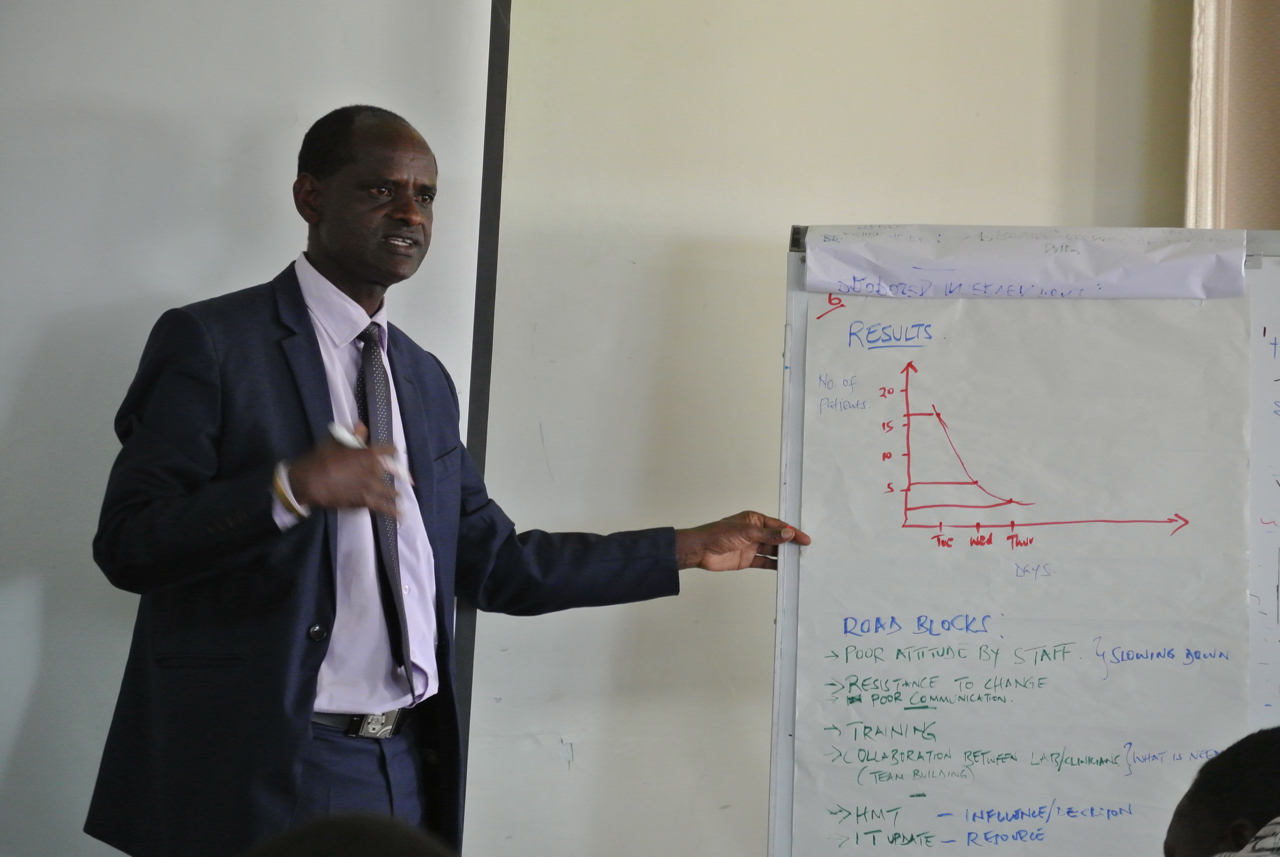
PROJECT 12. Reducing inpatient parenteral injections - including antibiotics
A nurse on a female surgical ward, although she was not yet fully trained, noticed that patients were remaining on intravenous antibiotics and other drugs for a very long time and that they remained unreviewed. The project which she and her team undertook was very successful. It is well described here on the poster that the team submitted to the International Forum on Quality and Safety in Healthcare in London in 2016.
SInce then , practice has improved considerably and has also had the impact of reducing outpatient injections (PROJECT 13) through increased awareness
PROJECT 13. Reducing outpatient parenteral injections
This team struggled to get this project off the ground; other outpatient projects were demanding time and triage has been prioritised for now.
PROJECT 14. Reducing unnecessary waits for lab tests
A lab in-charge, knew that patients often waited a long time in the queue for tests at his hospital, only to find that it wasn’t possible to do the test in the hospital that day. The project uncovered some very complicated processes and underlying problems. The team was diligent about meeting regularly, keeping meeting notes and trying different ways (using PDSA cycles) to improve the situation - which they have done! Keeping good notes to track progress is really helpful as most projects take some time to sort out.
Establishment of a different process and an additional paypoint at the lab, has resulted in much reduced time and fewer unnecessary waits.
PROJECT 15. Improving fasting times for adults waiting for surgery
A new fasting regimen has greatly reduced fasting times for patients and raised awareness among staff of how unpleasant it is to be deprived of food and drink while waiting for surgery.
PROJECT 16. Reducing cross-infection through better ward organisation
Staff on the female surgical ward recognised that cross-infection was inevitable because of traffic through a particular door and this was proven with an
excellent process mapping exercise and ward observation. They have reorganised where sterile supplies are kept on the ward and requested a swing door
to access sluice and toilets to avoid handling it.
PROJECT 17. Reducing waiting times in the out-patient/emergency department
Projects 4 & 5 were repeated in another hospital and many changes have been made. Engagement of staff who were not part of the Springboard programme remains a challenge but the team is determined to persist.
PROJECT 18. Improving resuscitation in the hospital
A healthy newborn baby requiring minimal resuscitation at birth died because equipment was not where it should have been and could not be found. Staff had the appropriate clinical skills and the equipment was in the hospital but there was no system in place for ensuring 24/7 availability at the point of need.
This is a tragic example of how system failure impacts directly on patient outcomes. The young doctor who was involved in this tragic situation was well trained - except in the skills to change the system.
"That workshop changed my perspective in so many ways; I am constantly trying to think of ways in which I could improve aspects of my work, my environment and even more. I have realized that just having that mindset is so key. Before I started working, I didn't realize the experiences I would go through, neither did I think I could make a difference to change set systems that others aren't comfortable changing. I was taught to treat during my education and not to focus on how best to do so. But now with some insight to hospital systems, I strongly believe I could mould a few minds to think beyond just set expectations in our career."
Young Doctor, reflecting on SPRINGBOARD programme (Project 18)
PROJECT 19. Improving communication
This lovely team recognised that they were having communication difficulties as their work expanded. A good open discussion and an analysis of the different elements of communication enabled them to tackle this problem and build the team up again.
They used the ‘fishbone’ tool to unpick the different elements of the communication issue so and this enabled them to rapidly address them. Among other things they established a group WhatsApp and daily early briefing meetings before the day’s work. They also established a QI committee to ensure ongoing progress.
PROJECT 20. Improving clinic flow
Flow within all hospital settings is a challenge. The team at Kwale Eye centre wanted to know if they could improve their flow and reduce waiting times in their clinic. First of all the current state was plotted.
They ran a fantastic live project plotting and timing the patient journey with expert Kate Silvester - the paper resulting from this (Roberts HE, Silvester KM. Finding the constraints in an ophthalmology clinic. Journal of Improvement Science 2017; 45: 1-21) was published in the Journal of Improvement Science. https://www.improvementscience.co.uk/jois/jois_view_abstract.php?volume=45
HOW WE WORK
q4a principles of practice:
we only work with people who want to work with us
empowerment of the people we work with lies at the heart of what we do
we always take a patient-centred approach
we always work in the spirit of partnership & co-creation
training of local trainers/coaches is integral to our approach
we work on a not-for-profit basis
How does q4a fit into the QI landscape?
q4a has the expertise and experience to support the development of QI & Leadership skills locally and globally. Since the development of the SPRINGBOARD course, three international reports on quality of care have been published, emphasising the need for just these skills.
These reports are:
The Lancet Global Health Commission:
High-quality health systems in the Sustainable Development Goals era: time for a revolution (2018)
https://www.thelancet.com/pdfs/journals/langlo/PIIS2214-109X(18)30386-3.pdf
-
Delivering quality health services:
A global imperative for Universal Health Coverage (2018) from the World Bank, WHO and OECD.
-
Crossing the Global Quality Chasm:
Improving Health Care Worldwide (2018): A Consensus Study Report published by the National Academies of Sciences, Engineering & Medicine
https://www.nap.edu/catalog/25152/crossing-the-global-quality-chasm-improving-health-care-worldwide
The First Lady of Kenya, Margaret Kenyatta and a Commissioner of the Lancet Report, launched it in Nairobi in April 2019 along with officials from the Ministry of Health, stating publicly that Universal Health Coverage in Kenya must be accompanied by high quality care.
We are contributing to this agenda independently and through collaborations with the very small number of other organisations who are delivering similar training such as Jacaranda Health https://www.jacarandahealth.org/ and LVCT Health https://lvcthealth.org/
The empowerment of healthcare professionals to create positive change at the point of care is essential for this transformation. We are giving them the tools to empower them.
Each SPRINGBOARD course is a blend of theory and practice that allows participants to gain a real understanding of how to implement continuous quality improvement (CQI), learned through doing real QI projects in mixed cadre teams.
20-24 mixed cadre participants attend each course and establish 3-4 QI projects in teams.
SPRINGBOARD courses are delivered by a joint UK and Kenyan faculty; a total of 3-4 per course, drawn from the q4a team below. The intention is to develop a majority Kenyan Faculty through ‘training of trainers’ courses.
MEET THE TEAM
Dr Kerri Jones - q4a UK lead
Kerri worked clinically in Anaesthesia and Critical Care. As Associate Medical Director at Torbay Hospital, England, she established the Horizon Centre to drive quality improvement and innovation across the health community. She has been an advisor to three Dept of Health national improvement programmes in England aimed at improving service user engagement, outcomes and patient experience through reducing waiting times and creating better surgical pathways. She was a Specialist Advisor to the Care Quality Commission (CQC) and is Visiting Fellow at Exeter University participating in a €2million European Union Innovation Research project.
She has been working in Kenya since 2009 and leads the Laikipia-Torbay Partnership. She co-established and is a trustee of Future Health Africa (originally known as ‘Exploring Global Health Opportunities’). She has a Certificate in International Health Consultancy from the Liverpool School of Tropical Medicine. She lectures on innovation, quality improvement, health systems and International health, and is a founder member of the Global Health Collaborative at Plymouth University.
DR. MARY NDUTA KIBOTE, KENYA BASED TRAUMA TEAM LEAD
I wanted so much to be a doctor that I took myself to the Ukraine to study for 6 years (as there were limited opportunities in Kenya). Learning Russian and Ukrainian was a big challenge but I succeeded. The charity supported me and now I am back in Kenya trying to improve healthcare here.
Through my undergraduate, internship and now as a registered doctor in Kenya, working as a volunteer in this charity, I have learnt many new surgery skills and also how to be a good team player. The work I have done with Future Health Africa has really helped me increase my confidence to work independently with minimal supervision
I believe FHA is one of the world’s best charities as it provides a broad range of well-organised clinical approaches and experiences. It also leaves behind successful sustainable qualitative operation programs and management. I value the opportunity of working with such a charity.
Dr Timothy Panga - q4a KENYA lead
Timothy is a Clinical Pharmacist with hands-on experience in health leadership in the Kenya public sector. He is currently the Chief Executive Officer of Nanyuki Teaching and Referral Hospital in Laikipia County, Kenya. He has served as the Chief Officer of Health in the County Government of Laikipia. In that role, he also served as the secretary of the Chief Officers of Health Forum in Kenya. He was one of the first Springboard programme graduates and is a major advocate for the training. He is focused on ensuring that the initiated QI projects in the various Kenyan hospitals are completed and build the body of knowledge on QI in Kenya.
He has a deep interest in Quality Improvement and Patient Safety. He advocates for the establishment of a healthcare accreditation system in Kenya that incorporates Quality Improvement. He trained as a Patient Safety Officer with the Institute of Healthcare Improvement (IHI). Back in 2012, he undertook a Clinical Fellowship at the Joanna Briggs Institute in the University of Adelaide, Australia which involved building the capacity of Gertrude’s Children’s Hospital (Nairobi) to conduct clinical audits.
He is also passionate about building the capacity of Clinical Pharmacy services in Kenya. He is the founding director of the Centre for Pharmaceutical Excellence, a pharmacy consulting group in Kenya. He participated in the First International Masterclass on Paediatric Pharmaceutical Care at Evelina Children’s Hospital of the Guy’s and St. Thomas’ NHS Foundation Trust in 2011. He serves the Pharmaceutical Society of Kenya as its Projects Manager, as well as in the external relationships, partnerships and governance committee.
Ms Jane Pyle,
Springboard Design & Delivery -
Foundation & Advanced courses
Jane Pyle is the Senior Clinical Pharmacy Manager at Torbay & South Devon NHS Foundation Trust in England where she has worked since 1999. Her main area of clinical expertise is in Gastroenterology but she has also worked in Nutrition and Mental Health teams. She has special interests in education and patient safety and has wide experience in the UK secondary care and academic sectors.
Jane has led many successful improvement projects related to patient safety and is passionate about the potential that good improvement methodology has to make patients and healthcare workers’ lives safer & easier. Jane has contributed greatly to the Springboard curriculum development.
Music is another love and Jane is a Trustee of the music charity ‘Wren Music” which works creatively with individuals and communities, enabling thousands of people every year to engage with music using voice or instruments, through traditional and folk music. Jane sings in the Torbay Folk Choir.
Ms Penny Humphris,
Faculty Lead, Springboard Advanced Course
Penny joined the NHS in England as a graduate trainee and spent her long career in hospital and strategic management and leadership in the NHS. She spent ten years at Board level, with seven years as Chief Executive of a Health Authority. From 2001 – 2005, she was Director of the NHS Leadership Centre and worked on the establishment of the NHS Institute for Innovation and Improvement.
She also has experience in management consultancy, gained during a period of employment with KPMG, and is a qualified coach. She now runs her own coaching and consultancy business, especially focusing on leadership development. Leadership programmes have been delivered for clinical leaders from all professional backgrounds focusing on leading the transformation of services for patients. Areas of coaching include optimising personal performance, building a high performing team, developing positive relationships and delivering results. Penny developed the leadership components of the SPRINGBOARD programme.
Dr Kate Silvester,
Faculty Lead Springboard Foundation Course
Kate originally trained as an ophthalmologist in England and retrained as a manufacturing engineer. She has 20 years’ experience of transferring the principles of manufacturing process design and improvement to address the delays in emergency and elective patient flow. In 2009 to 2012, for The Health Foundation, she coached 2 NHS Trusts to demonstrate the impact of poor patient flow on death rates and cost and how to improve them. http://www.health.org.uk/publication/improving-patient-flow
Kate was appointed to the Faculty of the Institute of Healthcare Improvement in 2001 and an Honorary Associate Professor at the University of Warwick in 2006. She now works independently and with an international network of healthcare design and improvement practitioners. She is co-founder of the Journal of Improvement Science (JOIS) http://www.improvementscience.net/jois/
Dr Joanne Watson,
Faculty, Springboard Foundation Course
Joanne is an international expert in Quality improvement. She is the System Medical Director and a Consultant Physician at Torbay & South Devon Foundation Trust with a remit for Quality Improvement. In her previous consultant post at Musgrove Park Hospital Taunton, she set up and managed an Improvement Network promoting patient safety and patient experience through building the culture, capacity and capability of staff to deliver great care. She has a particular interest in developing patient experience to be a driving force within health services. She undertook a Quality Improvement Fellowship with the Institute of Healthcare Improvement (IHI) in the USA and also with the Health Foundation in the UK. She was the national Clinical Lead for the King’s Fund’s Patient and Family Centred Care Programme.
She helped to establish and deliver the first SPRINGBOARD programme in Kenya in 2015.
Dr Nick Roberts
Springboard Advanced course trainer
Nick’s background is as a general practitioner in the NHS for 25 years. In addition to this clinical role, he has worked for Health Education England, delivering medical education. More recently he led Clinical Commissioning in Devon as the Chief Officer. Currently he undertakes mentoring and coaching, supporting health colleagues.
In addition to his medical career, Nick has been involved in several aspects of voluntary work both at home and abroad.
In the UK he has led the development of a sports facility to encourage more people, especially children, to get involved in sport. While in Africa he has supported Families for Children Zambia to address the needs of vulnerable children living in poverty. He has also been involved in delivering a leadership programme in Kenya.
In his spare time, Nick cycles and is a keen member of Sustrans (a UK sustainable transport charity making it easier for people to walk and cycle) and he enjoys many activities with his wife and two grown up children.
Ms Suzanne Obudo
Springboard Foundation course trainer
Suzanne is a Clinical Officer in Anaesthesia at Kisumu County Hospital in Kenya where she is also the Quality Improvement coordinator. She was trained in Quality Improvement techniques by the Deutsche Gesellschaft fuer Internationale Zusammenarbeit (GIZ) who are supporting 3 counties in Kenya to understand and implement the Kenya Quality Model for Health.
She has introduced the ‘Lean Café’ to the hospital and coordinates the growing Work Improvement Teams. She is the first Kenyan Faculty member and is advising the SPRINGBOARD team on Kenyan strategy and on alignment of Springboard with the Kenya Quality Model for Health.
Christine Musee
Springboard Advanced course trainer
Christine is Assistant Chief Nurse (Nursing Standards & Research) at Kenyatta National Hospital in Kenya. She has diverse interests and skills including Leadership & Management Research, Monitoring & Evaluation, Nursing Care, Mentorship and Coaching. She is the Monitoring and Evaluation lead for Springboard’s sister programme GRASPIT which she helped move from UK to entirely Kenyan delivered. She teaches and trains trainers for BLS, ACLS, ETAT+, GRASPIT.
Christine also acts as a mentor and spokesperson in her community, successfully balancing her roles as a wife, mother, Christian leader and writer in the making. She is full of energy and is passionate about promoting effective communication both in her workplace and in her community. q4a is delighted to welcome her as the first Kenyan faculty member on the Springboard Advanced (Leadership) course.
Mr Tim Spring
With 5 years’ experience in the private sector and 5 years’ experience with the NHS, Tim has worked in a variety of operational management roles; he managed leisure centres in Exeter, led innovation and improvement for Public Health provider services in Torbay and service development at the Royal Devon and Exeter NHS Foundation Trust (RD&E) where he is now supporting the implementation of a state-of-the-art Electronic Patient Record as Organisational Development Change Manager.
Driven by a desire to solve complex problems and improve patient care, Tim has developed a strong interest in improvement and innovation, and has completed an MSc in Healthcare Management, Leadership and Innovation alongside the Improvement Science Practitioner programme. Tim has put this learning to use by developing Devon’s Flow Coaching Academy and designing an Outpatient Services improvement programme.
In his spare time, Tim runs a small exercise company delivering cardiac, cancer and stroke rehabilitation services across Devon. He is also a keen musician.
Dr Simon Knowles
Dr Simon Knowles was the originator of the concept of the Springboard programme and delivered some of our early courses. Simon has extensive experience of teaching leadership & quality improvement to healthcare professionals in the UK and Africa, working with the Royal College of Pathologists.
His medical career as a Pathologist has been spent equally between Australia and the UK. He was recently President of the Association of Clinical Pathologists in the UK and a non-Executive Director of Torbay & South Devon Clinical Commissioning Group, which buys health and social care for South Devon residents. He was a Specialist Advisor to the Care Quality Commission. Simon believes that staff satisfaction and patient satisfaction are inextricably linked.
Tropical Health and Education Trust (THET) www.thet.org
A UK based Trust that uses Health Partnerships as a process of supporting local communities and Ministries of Health in Africa.
THET managed the Health Partnership Scheme (HPS) from 2012-2017, a programme funded by the UK Department for International Development (DFID). The scheme aims to improve health outcomes for poor people in DFID priority and other low income countries by supporting health partnerships to deliver projects aimed at improving the skills and education of health workers. Future Health Africa and q4a’s SPRINGBOARD programme was successful in securing several grants from the HPS initiative.
EVALUATIONS
A THET funded evaluation of the SPRINGBOARD Programme can be downloaded by clicking here (docx 59kb).
Participant feedback - what do people say
We have gathered participant feedback from all our training. It has been overwhelmingly positive with 84% of participants have rated the course overall as excellent and 16% as good.
One medical intern , when I told her that her project had been shared in presentations, said:
“I am extremely happy to hear that you have been able to share my story to various crowds to help people understand the importance of good systems in place. It is the very least I could do. That workshop changed my perspective in so many ways; I am constantly trying to think of ways in which I could improve aspects of my work, my environment and even more. I have realized that just having that mindset is so key. Before I started working, I didn't realize the experiences I would go through, neither did I think I could make a difference to change set systems that others aren't comfortable changing. I was taught to treat during my education and not to focus on how best to do so”.
More participant feedback:
“....the place is more beautiful, you cannot compare with what we had before and some of the junk we were keeping - none of us can tell what we were keeping it for. Patient flow has been streamlined. Waiting time has definitely improved from hours to minutes…”
“I got to know that change begins with me and we do not need added resource for improvement.”
“It’s that feeling of ‘unblocking the drain’! The satisfaction is IMMENSE!”
“There is so much to do yet we do so little because of the thought that change can only be done by the bosses.”
“We all need the various skills in leadership, coaching, emotional intelligence - just what I was missing.”
NEWS, EVENTS & RESOURCES
This section contains links to external resources have informed our work. You can download out latest newsletter here (docx 949kb).
Reports on high quality care:
Three very important reports were published in 2018 emphasising the need for Universal Health coverage to be accompanied by higher quality care. These were:
The Lancet Global Health Commission: High-quality health systems in the sustainable development goals era: time for a revolution.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al.
Lancet Glob Health. 2018 Nov;6(11):e1196–252. (The Lancet Global Health Commission Sept 2018)
https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(18)30386-3/fulltext
Delivering Quality Services: A Global Imperative for Universal Health Coverage: OECH/WHO Report 2018
Read online at https://read.oecd-ilibrary.org/social-issues-migration-health/delivering-quality-health-services-a-global-imperative_9789264300309-en#page1
Crossing the Global Quality Chasm: Improving Health Care Worldwide.
National Academies of Sciences, Engineering, and Medicine 2018. Washington, DC: The National Academies Press. https://doi.org/10.17226/25152
Documents & Guides
PDF: Quality Improvement Made Simple – what everyone should know about healthcare quality improvement. Developed by The Health Foundation.
A Guide to Service Improvement ( NHS Scotland): https://www2.gov.scot/resource/doc/76169/0019037.pdf
The Quality Improvement Guide (NHS Wales) http://www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/Quality%20Improvement%20Guide%20-%203rd%20edition%20%28IQT%29%20WEB.pdf
Going ‘Lean’ in the NHS (Although this has ‘NHS” in the title, it is a useful general introductory guide to ‘Lean’ methodology)
The Royal College of Emergency Medicine in the UK has provided all their QI resources one webpage. This is all free to use and covers most aspects of QI. https://www.rcem.ac.uk/RCEM/Quality_Policy/Professional_Affairs/Research/Resources/RCEM/Quality-Policy/Professional_Affairs/Resources.aspx?hkey=23e863f7-00e1-41ef-97c0-b1a09c688635
Kenya Quality Model for Health (KQMH): A Training Course for the Health Sector
https://www.usaidassist.org/resources/kenya-quality-model-health-training-course-health-sector
Development of a national strategic framework for a high-quality health system in South Africa: https://www.hst.org.za/publications/South%20African%20Health%20Reviews/Chap%209%20Quality%20SAHR2018.pdf
Books / Journals:
African Health leaders. Making Change and Claiming the Future.
Edited by Francis Omaswa and Nigel Crisp. ISBN: 9780198703327
Journal of Improvement Science
https://improvement.nhs.uk/resources/journal-of-improvement-science/
British Medical Journal Open Quality
https://bmjopenquality.bmj.com
British Medical Journal: Quality & Safety
https://qualitysafety.bmj.com/
International Journal for Quality in Health Care | Oxford Academic
https://academic.oup.com/intqhc
Global Journal on Quality & Safety in Healthcare
Courses in Quality Improvement & Patient Safety (some free):
Foundations of Improvement Science in Healthcare (FISH) (UK
Simon Dodds & Kate Silvester https://www.saasoft.co.uk/index.php
University of Bath course on Quality Improvement in Healthcare (UK)
https://www.futurelearn.com/courses/quality-improvement
Open University (UK)
Institute for Healthcare Improvement (USA)
http://www.ihi.org/education/IHIOpenSchool/courses/Pages/default.aspx
Johns Hopkins University (USA)
https://www.hopkinsmedicine.org/armstrong_institute/training_services/eLearning/index.html
https://www.coursera.org/learn/patient-safety-systems-view
Harvard Medical School (USA)
https://online-learning.harvard.edu/course/improving-global-health-focusing-quality-and-safety
Organisations with an interest in quality improvement & leadership:
The Institute for Healthcare Improvement (IHI) http://www.ihi.org
The Institute for Healthcare Improvement (IHI), an independent not-for-profit organization based in Cambridge, Massachusetts, is a leading innovator, convener, partner, and driver of results in health and health care improvement worldwide.
The IHI together with Harvard University have developed a comprehensive online QI course: https://www.edx.org/course/ph556x-practical-improvement-science-harvardx-ph556x
International Society for Quality & Safety in Healthcare (ISQua)
The Lancet Global Health Commission on High Quality Health Systems in the SDG Era (HQSS Commission)
The HQSS Commission is a group of 30 academics, policymakers, and health system stakeholders from 18 countries. It reviews current knowledge, produces new empirical work, and offers policy recommendations - outlined in its 2018 report (see report 1 above)
https://www.hqsscommission.org
The Health Foundation (UK)
The African Centre for Global Health and Social Transformation (ACHEST) http://achest.org
The African Centre for Global Health and Social Transformation (ACHEST) is an initiative promoted by a network of African and international leaders in health and development. It is both an independent Think Tank and a network and is led by Prof Francis Omaswa.
Tropical Health Education Trust (THET) www.thet.org
Tropical Health Education Trust (THET) is the UK support organisation for Health Links between health institutions in Africa, Asia and elsewhere in the world, and their counterparts in the UK.
Horizon Centre – Torbay and South Devon NHS Foundation Trust
www.torbayandsouthdevon.nhs.uk/horizoncentre
The Horizon Centre is an exciting innovation, education and research facility based at Torbay Hospital, UK. The Centre predominantly serves the UK National Health Service workforce, providing a state of the art environment where people can explore new ideas, learn new techniques and reflect on clinical practice together
South West Global Health Collaborative
https://www.plymouth.ac.uk/research/global-health-collaborative
Placed within Plymouth University in SW England, the Collaborative brings together volunteers, educators and researchers to increase the impact of their global health work through collaboration.
The South West Academic Health Science Network www.swahsn.com
The South West Academic Health Science Network (SW AHSN) is based in the south west of England and is dedicated to improving health and care and driving innovation acceleration across the region.
Centre for Health Solutions – Kenya (CHS) https://www.chskenya.org
Centre for Health Solutions – Kenya (CHS) is an indigenous, not-for-profit organisation with in-depth understanding of the local context, utilising local expertise and strategic partnerships to ensure the implementation of evidence informed solutions and interventions to existing and emerging public health concerns.
Jacaranda Health https://jacarandahealth.org
Jacaranda Health is a Kenya-based social enterprise that combines business and clinical innovations to create a fully self-sustaining and scalable chain of maternity clinics. The clinics provide affordable, high-quality maternal and child health services to poor urban women. Jacaranda has been using QI methodology to improve its services and has a focus on patient centred care.
LVCT Health Kenya
LVCT has been pioneering QI training in Community settings in Kenya for many years. Most recent has been the SQALE project http://usaidsqale.reachoutconsortium.org/
Papers of possible interest:
Editorial: How could health care be anything other than high quality?
Tedros Adhanom Ghebreyesus Lancet Glob Health September 2018 http://dx.doi.org/10.1016/S2214-109X(18)30394-2
Editorial: Improving the quality of health care across the health system
Shamsuzzoha B Syed,a Sheila Leatherman,b Nana Mensah-Abrampah,a Matthew Neilsona & Edward Kelleya Bull World Health Organ 2018;96:799 http://dx.doi.org/10.2471/BLT.18.226266
Quality improvement made simple: What everyone should know about healthcare quality improvement
Health Foundation (Aug 2013)
https://www.health.org.uk/sites/default/files/QualityImprovementMadeSimple.pdf
Understanding organisational culture for healthcare quality improvement.
Mannion R, Davis H.
BMJ 2018;363:k4907
https://doi.org/10.1136/bmj.k4907 (Published 28 November 2018)
Quality Improvement – training for better outcomes (Academy of Medical Royal Colleges 2016)
How to get started in quality improvement
Jones B, Vaux E, Olsson-Brown Anna
BMJ 2019;364:k5408 doi: 10.1136/bmj.k5437 (Published 17 January 2019)